Gestational Diabetes or GDM for short, is a common condition that occurs during pregnancy, specifically diagnosed around the third trimester. It is the transient form of Diabetes Mellitus that some women may acquire during pregnancy.
Diabetes refers to a high level of blood glucose. Glucose is the major energy source of the body. It comes from the digestion of carbohydrates and is carried by the bloodstream to the body cells. However, glucose cannot enter the body cells on its own. To do so, it requires assistance from a hormone produced by the pancreas, called insulin.
Insulin induces the cells to take up glucose, thereby, removing it from the bloodstream. Diabetes happens when insulin is either deficient or not used effectively. Without insulin, glucose cannot enter the body cells. It stays in the bloodstream causing high blood sugar.
During pregnancy, a temporary organ is developed to connect the mother and the fetus, called the placenta. The placenta supplies the fetus with oxygen and nutrient, as well as produces a number of hormones that work to maintain pregnancy. Some of these hormones impair the action of insulin, making it less effective.
This insulin counteractive effect usually begins at about 20 to 24 weeks of pregnancy. The effect intensifies as the pregnancy advance and the placenta grows larger and becomes most prominent in the last couple of months. Usually, the pancreas is able to adjust by producing more insulin. But in some cases, the level of placenta hormones may become too overwhelming for the pancreas to compensate, and gestation diabetes results.
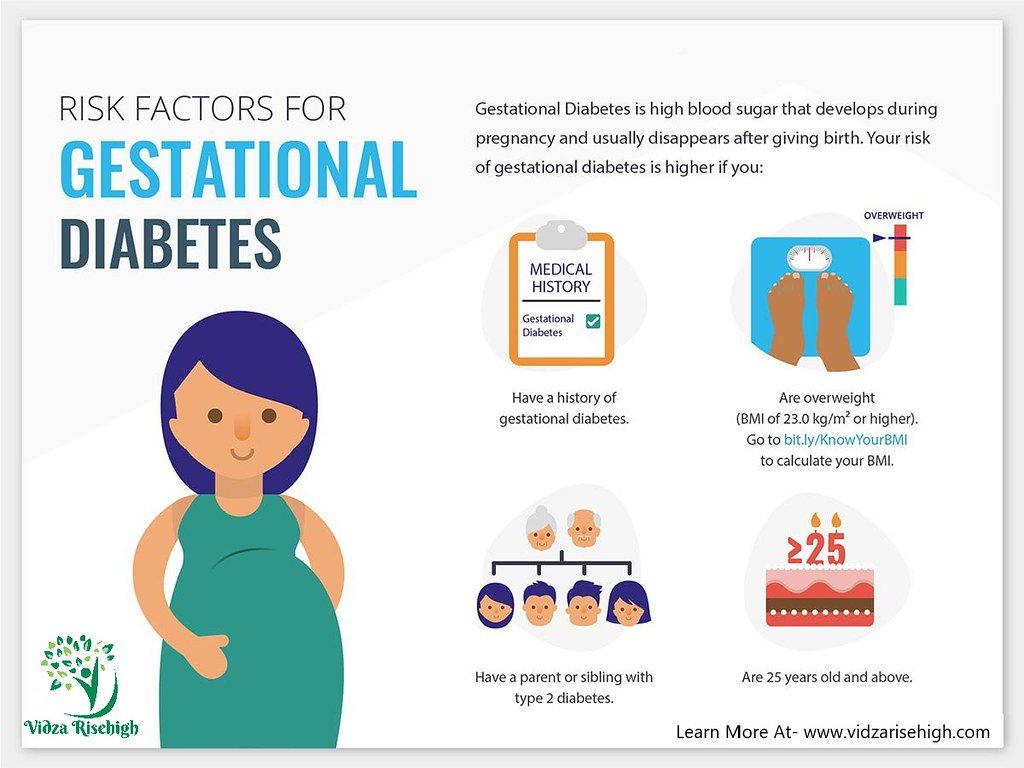
Any pregnant woman can develop gestational diabetes, but those who are overweight or obese, or have personal or family history of diabetes or prediabetes, are at higher risk. Other risk factors include age, race, and having previously given birth to large babies.

While gestation diabetes usually resolves on its own after delivery, complications may arise if the condition is severe and poorly managed. Because of the constant high glucose level in the mother’s blood, the fetus may receive too many nutrients and grow too large, complicating the birth process and a C-section may thus be required for delivery.

A high level of glucose may also stimulate the baby’s pancreas to produce more insulin than usual. And shortly after delivery, since the baby continues to have high insulin levels but no longer receives glucose or nutrients from the mother, the baby’s blood glucose level can drop suddenly and become exceedingly low (hypoglycemia) causing seizures. The newborn’s blood glucose level must therefore be monitored closely and be corrected promptly. High blood glucose levels may also cause a risk of preterm birth and future diabetes in both mother and child.

Gestational diabetes can be successfully managed or even prevented with healthy diets, physical exercise, and keeping a healthy weight before entering pregnancy. In some cases, however, oral medications or insulin injections may be needed.
REFERENCE
- https://mems.my/wp-content/uploads/2019/07/CPG_Management-of-Diabetes-in-Pregnancy.pdf
- https://mems.my/wp-content/uploads/2019/07/Diab-in-Pregnancy_Quick-Reference.pdf
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/diabetes/gestational-diabetes
- https://emedicine.medscape.com/article/127547-overview




